The New Standard of Care: Staff Safety
The surgical operating room (OR) remains the core of a healthcare institution, a meticulously controlled environment where skill, technology, and teamwork converge to save lives. Yet, within this sterile and precise space, a significant and persistent risk endures: sharps injuries.

Scalpels, needles, and other sharp instruments, while indispensable to surgical procedures, pose a considerable threat to every member of the surgical team. These injuries are far from trivial; they carry the potential for devastating consequences, including the transmission of bloodborne pathogens such as HIV, Hepatitis B, and Hepatitis C. Historically, safety protocols have been largely reactive, focusing on managing injuries after they occur. However, the current evolution in surgical practice demands a more proactive, comprehensive, and preventative approach, which is now emerging as The New Standard of Care for the operating room.
The Traditional Paradigm of Sharps Safety
The traditional paradigm of sharps safety was often predicated on individual vigilance and post-exposure prophylaxis. Surgeons, nurses, and operating room technicians were trained to exercise extreme caution, and in the event of an injury, to follow a strict protocol for reporting and medical follow-up. While a necessary component, this approach places the burden of safety almost entirely on the individual, failing to address the systemic and environmental factors that contribute to these incidents.

The high-pressure, fast-paced nature of the OR, combined with the inherent complexity of surgical procedures, creates an environment where human factors like fatigue and miscommunication can lead to catastrophic accidents. The most common incidents—an errant scalpel left on a tray, a needle passed without clear communication, or a misplaced suture needle—are frequently products of these systemic vulnerabilities rather than a simple lapse in individual judgment.
Embracing a Comprehensive Safety Strategy
To move beyond this reactive stance, surgical institutions are now embracing a comprehensive safety strategy that integrates technology, protocol, and a robust safety culture. This begins with the widespread adoption of safety-engineered devices. The use of single-handed scalpel blade removers, blunt-tip suture needles, and hands-free transfer zones for sharps are becoming industry standards. These innovations physically mitigate the risk of injury.
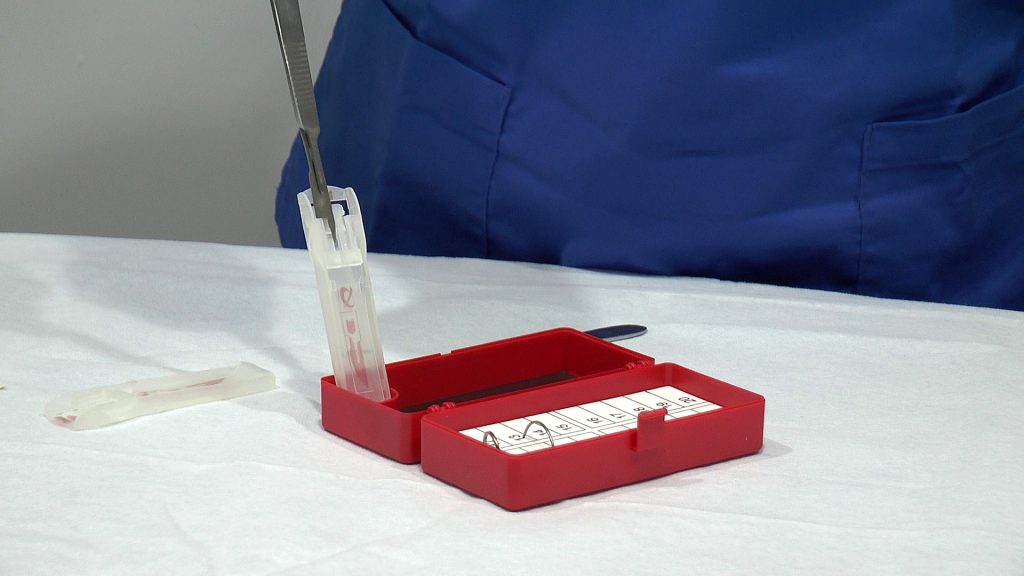
Furthermore, standardized protocols for sharps management, such as the use of dedicated sharps containers at every workstation and the implementation of a neutral zone for instrument passing, have been shown to significantly reduce the incidence of injuries. These technological and procedural changes are no longer merely recommendations; they are becoming the cornerstone of a safe surgical environment.
The New Standard of Care
These changes represent a cultural transformation that establishes staff safety as The New Standard of Care. It is a recognition that safety should be required for both staff and patients.
This cultural change involves fostering an environment of psychological safety where team members feel empowered to speak up about risks, near misses, or observed unsafe behaviours without fear of reprisal. A team-based approach, where every member—from the surgeon to the circulating nurse—is actively involved in anticipating and mitigating risks, is essential. Regular huddles before and after cases, clear communication protocols, and simulation-based training can help reinforce these behaviours.

By prioritizing the mental and emotional well-being of the surgical team, institutions can reduce fatigue and stress, thereby enhancing cognitive function and lowering the likelihood of error. This holistic perspective acknowledges that a safe and supported team is the most reliable predictor of a safe and successful patient outcome.
Sharps safety in the operating room have evolved from a matter of individual caution to a systemic, multi-faceted mandate. By combining safety engineered devices, standardized protocols, and a cultural commitment to proactive safety, the healthcare industry is moving towards a new paradigm. This approach, which holistically protects the well-being of the surgical team, represents The New Standard of Care. It is a powerful acknowledgment that the safety of the provider is inextricably linked to the quality and safety of the care delivered to the patient. Embracing this standard is not only an ethical obligation but a strategic imperative for every institution committed to excellence in surgery.

